Cannabis has been used as medicine for thousands of years across the globe. It was only in the early 20th Century that regulations were put in place to classify it as an illegal substance in the United States. Cannabis was officially outlawed at the federal level in the US in 1970. With the passage of California’s Proposition 215 in 1996, cannabis for medical use has become increasingly popular. In 2012, states in the US began to legalize cannabis for recreational use. Today, there is more and more research being done to fully understand the medical and health benefits of cannabis.
For the cancer patient, cannabis has a number of potential benefits, especially in the management of symptoms. Many scientists and doctors tout the benefits of cannabis in managing the side effects of chemo and radiation therapies such as nausea, vomiting, pain, insomnia, and depression. The patients we are in contact with, often share how cannabis has helped them with various symptoms during and after treatment.
In a study presented at the 2019 annual meeting of the American Society for Clinical Oncology (ASCO), it was revealed that an overwhelming majority of oncologists strongly support and recommend the use of medical marijuana for cancer patients. The problem is that almost half of them feel they are not qualified to prescribe it as part of the treatment.
Dr. Noah Federman, who was first connected with the Hirshberg Foundation via the 3rd Annual UCLA Cannabis Research Symposium in 2019, specializes in cannabis and oncology. His clinical oncology practice uses cannabis and cannabinoid compounds as adjunctive therapies and has a keen interest in how they can help patients. After hearing his academic lecture on “Cannabis Use in Oncology” it was clear our pancreatic cancer community would benefit and appreciate hearing him present the latest information. Dr. Federman will share the science behind the anecdotal stories in this ever-emerging field.
Watch Webinar
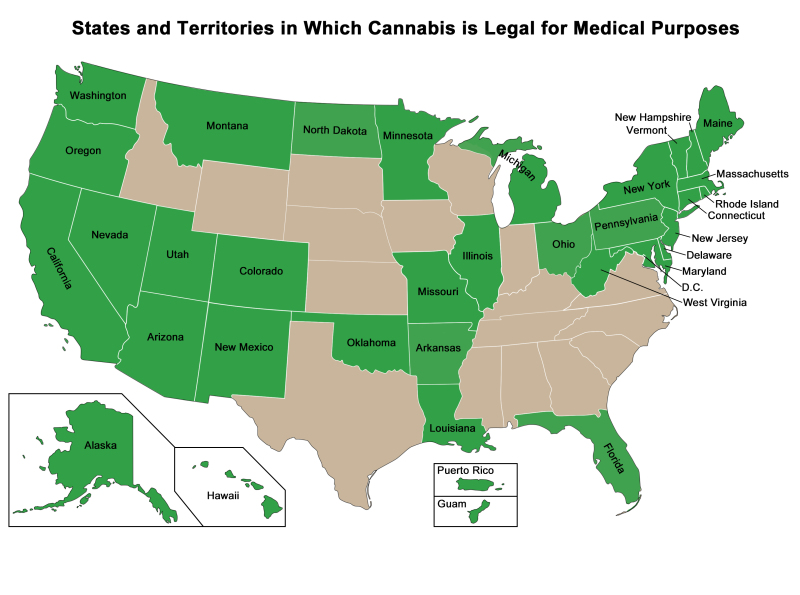
The NIH (National Institute of Health) has created a map showing the U.S. states and territories that have approved the medical use of cannabis. Last updated: 03/23/2020
In addition to Dr. Noah Federman’s position as Director of the Pediatric Bone and Soft Tissue Sarcoma Program at UCLA, he is a faculty member of the UCLA Cannabis Research Initiative. The UCLA Cannabis Research Initiative(UCLA-CRI) is one of the first academic programs in the world dedicated to the study of cannabis.


