One of the main ways to improve the outcomes for pancreatic cancer patients is early diagnosis and the way to better diagnostics is through a greater understanding of the initiating events in tumor progression. That is exactly what Kathleen DelGiorno, Ph.D. and her lab at Vanderbilt University are studying.
Dr. DelGiorno was a 2018 Seed Grant Awardee back when she was at The Salk Institute for Biological Studies in the Wahl Lab. Thanks to funding from the Hirshberg Foundation, she was able to publish her research, collaborate on other publications, and in her words, “become a much more attractive candidate for Assistant Professor positions.” We were thrilled to hear that in July 2020 she was offered the position of Assistant Professor at Vanderbilt University in Nashville, TN. She wrote to Agi, “Your generous funding has allowed me to be very productive over the last year. Thank you so much for launching my career!” Dr. DelGiorno’s success is emblematic of what our Seed Grant program aims to achieve.
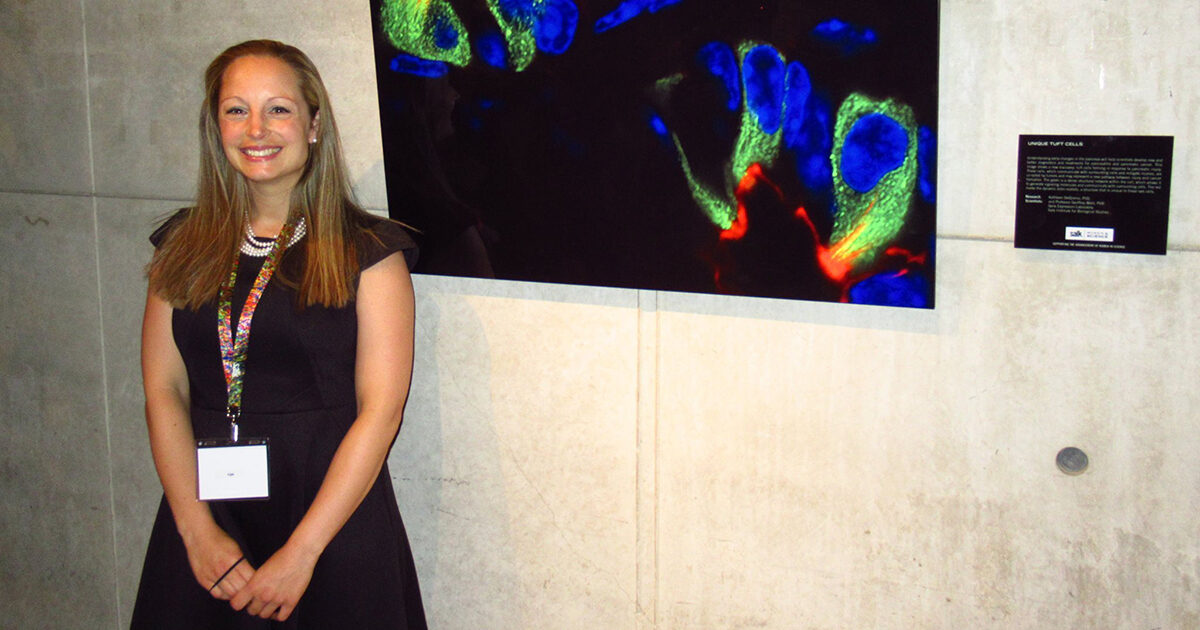
Below, read more about Dr. Kathy DelGiorno’s research and what she has been studying thanks to support from the Hirshberg Foundation.
Dr. DelGiorno’s research is looking to uncover early changes in the pancreas that lead to tumor formation. Chronic pancreatitis is a known risk factor for pancreatic ductal adenocarcinoma (PDAC), which accounts for more than 90% of pancreas cancers, and is characterized by inflammation, fibrosis and acinar to ductal metaplasia (ADM). ADM is a process where acinar cells (differentiated specialized cells in the pancreas) undergo remodeling back to ductal-like cells when the pancreas is injured. When oncogenic KRAS is present, ADM can be initiated, but the reversal of ADM does not happen, leading to metaplastic cells (less differentiated cells) that can then lead to precancerous lesions such as pancreatic intraepitheliel neoplasia (PanINs) or directly into PDAC. Dr. DelGiorno also studies tuft cells, which are solitary chemosensory cells seen throughout the hollow organs of the digestive tract and have been found to form spontaneously in the pancreas as the result of injury or tumorigenesis.
Research published by Dr. DelGiorno in Frontiers in Physiology details the landmark formation of tuft cells in the pancreas of wild-type mice, those with no genetic mutations, in the context of wound healing. This study linked tuft cell formation to ADM and shows that ADM takes place in the pancreas of mice after injury. This research demonstrates that wild-type mice can be used as a model and establishes a system to further study pancreatic tuft cells.
Subsequent research published in Gastroenterology, demonstrated that the formation of tuft cells originated during ADM, and that tuft cell generation may be a step in the process of tumorigenesis in the pancreas. The study found that when tuft cell formation was inhibited, pancreatic cancer development increased. They analyzed gene expression and found differences in the genes involved in inflammation, lipid (fat) synthesis, and metabolism. Prostaglandins, lipids that have hormone like functions, specifically prostaglandin D2, was shown to be lower when tuft cells were deleted. These lipids play an important role in keeping the pancreas from becoming inflamed and activating stromal cells, which contribute to pancreatic tumor formation. This suggests that tuft cells may actually restrain early tumor progression by secreting lipids, which inhibit inflammation.
Recently, Dr. DelGiorno’s lab at Vanderbilt released a pre-print (a research paper that is still under peer review) at bioRxiv using single cell sequencing to characterize all of the cell types that result from ADM and pancreatic injury. They found that, in addition to tuft cells, ADM is also characterized by enteroendocrine cell formation, cells that generate hormones with the potential to control information, tissue injury, and tumor formation. The DelGiorno lab is now studying how these cells control tumor formation and their potential to become tumors themselves.
Through her lab at Vanderbilt, Dr. DelGiorno’s research continues studying how tuft cells inhibit tumors in the hopes that these pathways can be mimicked therapeutically. Her ultimate goal is to exploit anti-tumorigenic signaling or target pro-tumorigenic signaling pathways in the hopes of benefitting patients. We applaud the work of Dr. DelGiorno and her lab for their contributions to understanding the early mechanics of tumor formation.
These advances are made possible thanks to your support. Thank you for helping us fund this vital research.